What Is Functional Endoscopic Sinus Surgery (FESS)?
Functional endoscopic sinus surgery (FESS) is a minimally invasive procedure used to treat chronic sinus problems that don’t improve with medication or other non-surgical treatments. During FESS, a surgeon uses a thin, flexible endoscope with a camera to visualize the nasal passages and sinuses, enabling precise removal of blockages, such as inflamed tissue, polyps, or bone. By restoring normal sinus drainage and ventilation, FESS helps relieve symptoms like nasal congestion, facial pressure, and sinus infections.
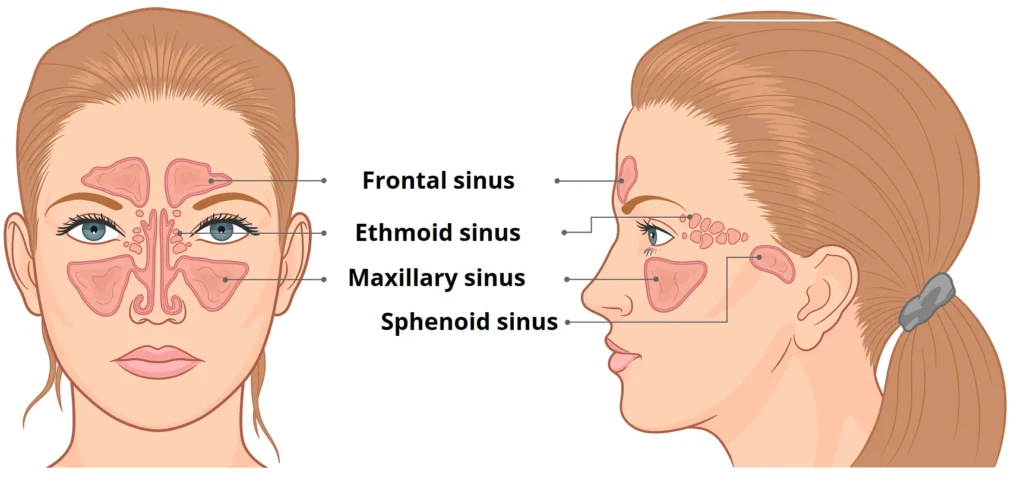
- Ethmoid sinus
- Frontal sinus
- Maxillary sinus
- Sphenoid sinus
FESS and Persistent Sinus Issues
During FESS, the surgeon carefully opens blocked sinus passages, removes inflamed tissue or polyps, and restores normal drainage and ventilation. This approach not only alleviates current symptoms but also reduces the likelihood of recurrent sinus infections. For patients with chronic sinusitis, FESS often provides long-lasting relief when non-surgical treatments have failed.
History of FESS
FESS was pioneered by Professors David Kennedy, Walter Messerklinger, and Heinz Stammberger in the United States and Austria. The development of endoscopes with light sources and cameras enabled surgeons to visualize and access the sinuses through the nasal passages, leading to the emergence of FESS as a safer, more effective alternative to open sinus surgery.
Benefits of Functional Endoscopic Sinus Surgery
1. Minimally Invasive
2. Improved Visualization
3. Preservation of Normal Anatomy
4. Customized Treatment
5. High Success Rates
6. Reduced Nasal Congestion
General vs Local Anesthesia: Which Option Is Better for FESS
For FESS, both general and local anesthesia can be used, but general anesthesia is often preferred for endoscopic procedures. It ensures that patients remain completely still and comfortable during surgery, allowing the surgeon to work precisely within the delicate sinus passages. While local anesthesia with sedation may be an option for less extensive cases, general anesthesia provides optimal conditions for thorough and safe treatment, particularly when multiple sinus cavities need to be addressed.
FESS Recovery
Recovery after FESS is generally smooth because it is a minimally invasive surgery. FESS is usually performed as an outpatient procedure. Patients typically spend a short time in the recovery room before going home, with some postoperative discomfort expected, including mild pain and bloody discharge from the nose.
Pain medication can help manage any soreness, while nasal saline sprays and sinus irrigation are essential for keeping the nasal passages clean and promoting healing. Nasal steroids and nasal sprays may be prescribed to reduce inflammation, and patients are advised to avoid nose blowing during the initial healing period. In some cases, temporary nasal packing is used to control bleeding, but most patients experience gradual relief as the sinuses recover.
Contact Our Healthcare Providers at Texas Sinus & Snoring
I started Texas Sinus & Snoring because there is a link between snoring and nasal obstruction. One common finding in evaluating the nose for obstruction is chronic sinus inflammation. Although I often alleviate this inflammation with antibiotics or balloon sinuplasty, I am also an expert at functional endoscopic sinus surgery (FESS).
Functional endoscopic sinus surgery has revolutionized the treatment of chronic sinusitis and other sinus disorders, offering patients a minimally invasive and highly effective surgical option. By restoring normal sinus function and addressing the underlying causes of sinus disease, FESS can significantly improve symptoms and quality of life for many patients. However, patients need to be well-informed about the benefits, risks, and potential complications associated with FESS.
Our surgeons approach each case with meticulous care and attention to detail, ensuring the best possible outcomes for our patients. Through ongoing research, technological advancements, and continued refinement of surgical techniques, the field of functional endoscopic sinus surgery continues to evolve, offering hope of improved outcomes and quality of life for patients with chronic sinus disorders.
Deviated Nasal Septum: Its Effects on the Frontal Sinus and Inferior Turbinates
A deviated nasal septum can have a significant impact on sinus function and nasal airflow, particularly affecting the frontal sinuses and inferior turbinates. When the septum is off-center, it can obstruct the natural drainage pathways of the frontal sinuses, leading to chronic sinus pressure, congestion, and recurrent infections.
In addition, a deviated septum often forces the inferior turbinates to compensate by swelling or enlarging, further narrowing the nasal passages and exacerbating breathing difficulties. This combination of septal deviation and turbinate hypertrophy can contribute to persistent nasal obstruction, snoring, and decreased oxygen flow, making surgical correction through septoplasty or FESS a critical option for restoring normal sinus function and improving overall nasal airflow.
Correcting a Deviated Septum with FESS and Septoplasty
Combining FESS with Endoscopic Orbital Decompression (EOD)
Conclusion
Functional endoscopic sinus surgery offers a safe and effective solution for patients struggling with chronic sinus problems. Using nasal endoscopy, surgeons can carefully evaluate the nasal cavity and identify conditions such as nasal polyps, bacterial infections, or obstructions in the ethmoid air cells. Procedures like ethmoid sinus surgery and endoscopic decompression target these areas, including the lateral nasal wall, to restore normal sinus drainage and improve breathing.
While FESS is generally safe, potential complications, such as cerebrospinal fluid leaks, must be considered, underscoring the importance of experienced head and neck surgery specialists. Addressing underlying sinus problems with these minimally invasive techniques allows patients to experience long-term relief, improved nasal function, and better overall quality of life.