Pages
- Podcast
- Genio Sleep Therapy
- Thank You
- Vendor Interest Form
- Health Fair
- Allergies Landing Page
- Test
- Sleep Apnea Landing Page
- Sinus Surgery landing
- Privacy Policy
- Accessibility
- Terms And Conditions
- Blog
- Home
- Sinus Quiz
- Injection Snoreplasty
- Snoring
- Uppp
- Oral Appliances
- Nasal valve reconstruction
- Inspire sleep therapy
- At home sleep study
- Airlift
- Sleep Apnea
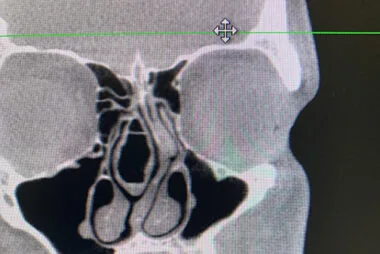
- Septoplasty
- FESS
- Balloon Sinuplasty
- Sinus Surgery
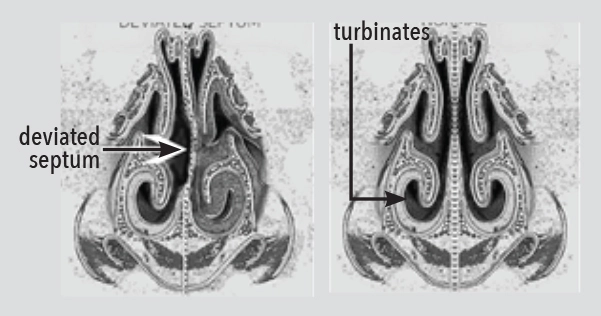
- Turbinate Reduction
- Rhinoplasty
- Clarifix Cryotherapy
- Nasal Breathing
- Hearing Aids
- Eustachian tube dilation
- Audiology hearing tests
- Hearing
- Immunotherapy
- Allergy Testing
- Allergies
- Services
- Reviews
- Insurance
- Tinnitus
- Snoring
- Sinusitis
- Sinus Headache
- Nasal Congestion
- Deviated Septum
- Chronic Rhinitis
- Chronic Cough
- Allergies
- Conditions
- Team
- Office
- About